Top Rated Dentists
Welcoming All New Patients
Welcoming All
New Patients
Welcome to Bloomfield Dental Associates where Dr. Dheeren Padhiar and his experienced team are committed to excellence in compassionate and gentle dental care. At Bloomfield Dental we specialize in preventative, restorative, and cosmetic dentistry.
Welcome to Bloomfield Dental
Complete health may be our long-term goal, but our immediate priority is the patient comfort. We do our best to facilitate a relaxing and non-threatening office environment you’ll want to return to again and again. This includes the implementation of multiple techniques to prevent treatment discomfort and minimize anxiety.
Office Tour
Come take a look inside.
Testimonials
Read reviews from our patients.
Smile Gallery
View real results from real people.
Bloomfield
Smile Membership
It is extremely important to maintain a healthy mouth and it is always our goal to preserve your natural teeth. We now offer Smile Memberships. A white, bright beautiful smile is now accessible to anyone, as our team has the skill, experience, and knowledge to create it for you. With the Bloomfield Smile Membership Plan, everyone can have a healthy smile.

Bloomfield Smile Membership
It is extremely important to maintain a healthy mouth and it is always our goal to preserve your natural teeth. We now offer Smile Memberships. A white, bright beautiful smile is now accessible to anyone, as our team has the skill, experience, and knowledge to create it for you. With the Bloomfield Smile Membership Plan, everyone can have a healthy smile.
Creating Healthy Smiles
Featured Services
We know our patients have a choice in several different areas, so we go out of our way to deliver the level of care and compassion we would want for our own families.
Meet Our Experienced Team
Compassionate Care
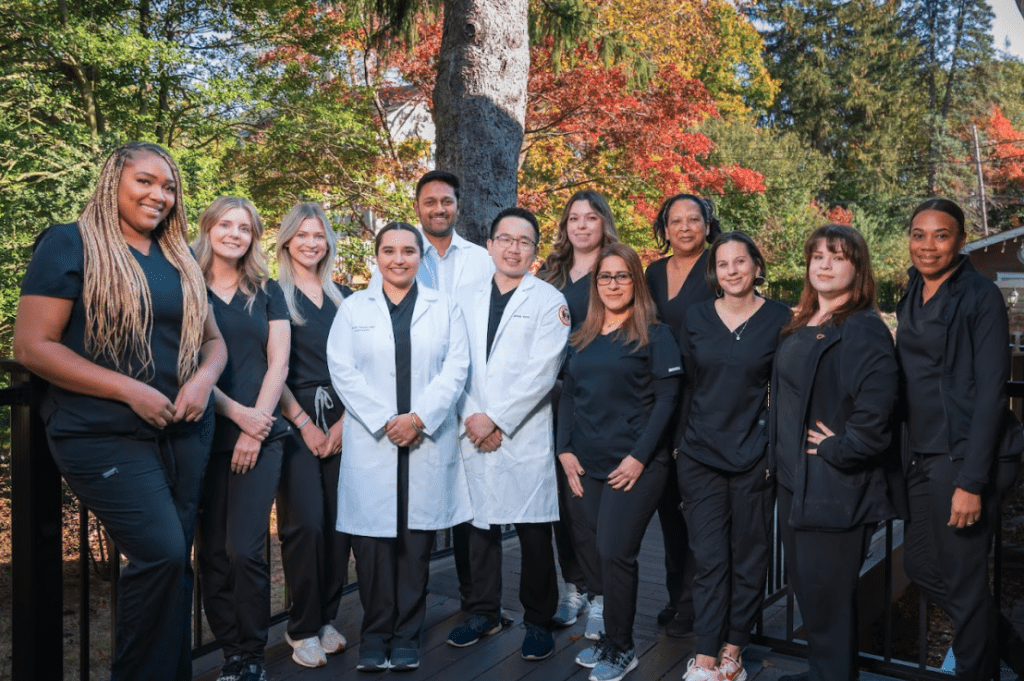
We know that the heart of this practice is the patients. Since we are a small, doctor owned family office, Dr. Dheeren and his team of dentists are better able to provide personalized care, with higher quality service. This helps him and his team build good relationships with their patients, which fosters a spirit of trust that is invaluable to us. Our dentists were recently awarded Top Dentist for Pennsylvania, a prestigious award that demonstrates our competence and care. We are delighted to get to know you and your family and continue to bring you exceptional, comprehensive dental care in Drexel Hill, PA for years to come.
Why Choose Us?
We know there are many dental offices to choose from, and we are honored that you have chosen ours. We do not take our responsibility to you lightly and we will work very hard to earn your complete satisfaction.
- Hablamos Espanol
- Award-Winning
- Exceptional Quality
- Over 100+ Google Reviews
- Online Appointments
- Advanced Technology
- Insurance Compatibility
- Affordability



